Pakistan Gamma Knife
In keeping with the tradition of innovation, NCCI in the year 2008 became the first medical institute in Pakistan to have a Gamma Knife & X Knife Radiosurgery System installed. This is one of the 400 Gamma Knife Radiosurgery units installed worldwide.
NCCI has installed the;
- Leksell Gamma Knife® ICON™
- A state of the art and revolutionary gamma knife unit capable of unprecedented precision and accuracy in radiation treatment delivery irrespective of the method of immobilization. ICON™ is also equipped with the Leksell Gamma Plan, a premier and flagship treatment planning system with enhanced new features.
Some of the finer points and answers to frequently asked queries are
- In Gamma Knife procedures there are NO incisions.
- Gamma Knife is not an actual knife.
- Gamma Knife Radio-Surgery is a completely PAINLESS & BLOODLESS procedure.
How is Gamma Knife radiosurgery different from other radiosurgery devices;
- Lower dose to Normal Brain Tissue
- Lower dose to the Body
Gamma Knife Radiosurgery (GKRS) is a precise and powerful treatment for brain disorders. It is noninvasive, effective and safe. This makes it the optimal choice for treating a wide variety of conditions including benign or malignant brain tumors, blood vessel malformations, trigeminal neuralgia and tremor disorders.
Gamma Knife can be used for both children and adults who meet the criteria for treatment with this advanced technology.
It is a method of radiosurgery that delivers extremely focused beams of cobalt radiation to precise targets in the brain – as many as 192 individual beams. Individually, the beams are too weak to damage healthy tissue. Together, they converge to deliver powerful treatment to a single point.
Another term for this type of noninvasive neurosurgery is “stereotactic” radiosurgery. This refers to directing radiation to a specific focal point using an external, three-dimensional frame of reference — such as the head frame used in Gamma Knife radiosurgery.
There are many benefits to Gamma Knife radiosurgery. Hundreds of patients safely undergo Gamma Knife radiosurgery each year. The method has been used worldwide since 1968.
Gamma Knife radiosurgery allows patients to quickly return to their normal routines. In most cases, only a single procedure is necessary.
In addition, radiosurgery is less expensive than conventional neurosurgery. It eliminates the need for lengthy hospitalization, medications and rehabilitation.
What to Expect During Gamma Knife Surgery
Our experienced Gamma Knife team provides patients with maximum safety and efficacy. Skilled pre-treatment planning and the radiation’s focused delivery method lead to improved patient outcomes, enhanced quality of life and virtually nonexistent damage to healthy brain tissue.
Your physician and our Gamma Knife team members will discuss the radiosurgery with you before the procedure takes place. Since Gamma Knife radiosurgery is noninvasive, it is not necessary to shave or cut your hair.
During Radio-Surgery
Gamma Knife radiosurgery planning and treatment are performed on the same day. Treatment includes three phases: fitting the head frame, procedure planning and actual procedure.
Fitting the Head Frame
One of the key components in Gamma Knife radiosurgery is what is called the stereotactic head frame. The frame allows the physician to accurately pinpoint the area within your brain that will be treated. The frame is lightweight and attaches to the head with four screws, which ensures that the radiation beams are precisely directed to the target. In addition, the frame prevents the head from moving during imaging and treatment. A local anesthetic will be applied where the screws are to be attached.
Once the head frame is in place, images will be taken of your brain. This imaging may include magnetic resonance imaging (MRI), computed tomography (CT) or angiography. Imaging will determine the exact size, shape and position of the target within your brain.
Radio-Surgical Planning
The next stage is radiosurgical planning. Once the images have been taken, you are allowed to rest while the Gamma Knife physicians develop a precise radiosurgical plan. The plan is made using a specially designed computer that helps calculate how the radiosurgical procedure should be performed. This generally takes one to two hours. During this time, you can rest, watch television, read and use the restroom. The stereotactic head frame will remain attached.
Radio-Surgical Procedure
Once the radiosurgical plan is completed, the actual radiosurgical procedure can begin. You will lie down on the procedure couch and the head frame will be attached to a helmet. You will be awake throughout and will be able to communicate with the Gamma Knife team through an audio and video connection. We will be monitoring you at all times.
The procedure is silent and painless.
The procedure time will last a few minutes to more than an hour, depending on the size and shape of the targeted area.
After Radio-Surgery
Most patients should be able to return to their normal routines within a day or so. Some patients may be required to lie quietly for several hours after treatment or stay overnight for observation.
Risks and Outcomes of Gamma Knife Surgery
Follow-up is key when you’ve had Gamma Knife radiosurgery. That is because the effects of the radiosurgery occur over a period of weeks or months. Treatment is designed to stop the growth of tumors or lesions over a period of time. It is important that you stay in contact with your physician to determine progress of your treatment. This may involve follow-up imaging such as MRI, CT or angiography.
Some patients may experience a mild headache or minor swelling where the head frame was attached. This should resolve spontaneously.
Our Team
The experts in our Gamma Knife Stereotactic Radiosurgery Center have more than 15 years of combined experience in radiosurgery. Our team members are dedicated towards providing patients with optimal treatment options and strive to obtain satisfactory results. The following are the trained consultants that deal with all Gamma Knife procedures at NCCI.
- Professor A. Sattar M. Hashim, MBBS, MD, PhD.
Consultant Neurosurgeon & Neuro-Oncologist
- Dr. Aurangzeb Abbasi, MBBS, FCPS (SN)
Consultant Neurosurgeon & Neuro-Oncologist
Apart from these consultants we have a very well-trained ancillary staff in the Gamma Knife Suite at NCCI that make sure that your stay at the center is as pleasant as possible.
Common Diseases Treated with Gamma Knife Radiosurgery:
- Brain metastases, most commonly from lung cancer, melanoma, breast cancer, colon cancer, renal cell cancer, and gynecological and genitourinary cancers
- Benign brain tumors such as meningiomas, acoustic neuromas (i.e., vestibular schwannomas), and pituitary adenomas.
- Malignant (Cancerous) Brain Tumors
- Arteriovenous Malformations
- Trigeminal Neuralgia
- Intraocular Melanoma
- Head and Neck cancers, such as Nasopharyngeal Carcinoma
- Recurrent Malignant Primary Brain Tumors
- Glomus Jugulare Tumors
- Essential Tremor (Thalamotomy with Gamma Knife)
RESULTS OF SOME GKRS TREATED PATIENTS AT NCCI IN THE PAST 5 YEARS
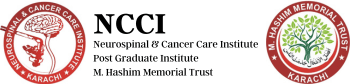
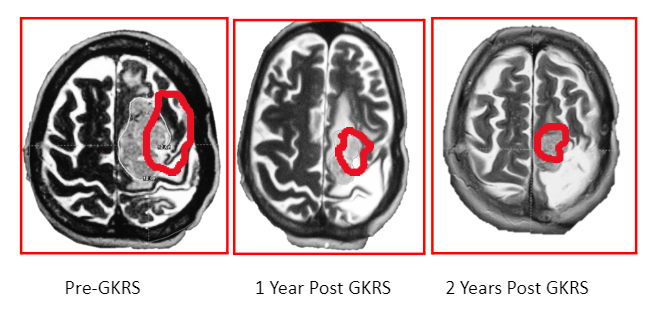
- GKRS FOR VESTIBULAR SCHWANNOMAS:
-
- Total Number of Cases: 394
- Interval Regression of Tumor: 316/394.
- Subtotal or Partially Excised: 70 (17%)
- First Line of Treatment: 324 (83%)
- Size Range: 34.2 to 28.7mm (median vol 12.85cm3)
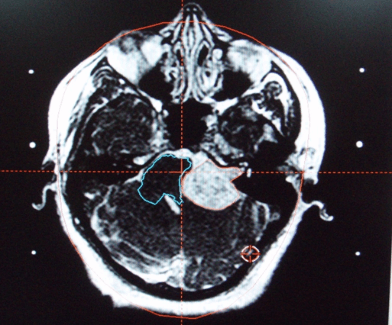
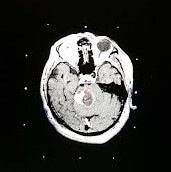
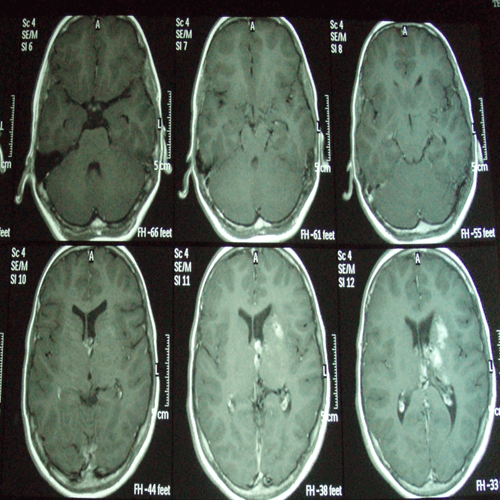
Pre-GKRS
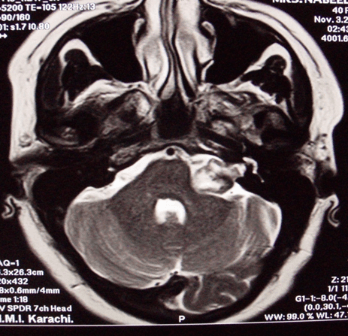
1 Year Post GKRS
6 Months Post GKRS
PATIENT 2
2012
2013

2014

2015

2016
- GKRS FOR MENINGIOMAS
-
- Total Number of Cases: 378
- Residual/Recurrent Lesions: 117
- Primary Treatment: 217
PATIENT 1
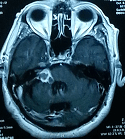
Pre-GKRS
12 months Post GKRS
PATIENT 2
RESULTS:
- Follow Up Period was 52 Months
- Interval Regression of Tumor: 220/378
- Interval Stable Tumor: 78/378
- Interval Progression of Tumor: 08/378
- Majority were Skull Base Lesions: 62%.
- Follow up period: 52 months in 320 pts.
- Complications: 14 pts (4.2%)
- fits
- transient cranial neuropathies
- symptomatic edema.
- GKRS FOR CRANIOPHARYNGIOMAS:
- Total patients 75
- Age range 2 – 53 years (mean 20)
- Subtotal resected 11 (14.6%)
- Neuroendoscopic fenestration 2 (2.6%)
- VP shunt placed 27 (36%)
- Ommaya reservoir placed 10 (18.3%)
- Conventional radiotherapy 4 (5.3%)
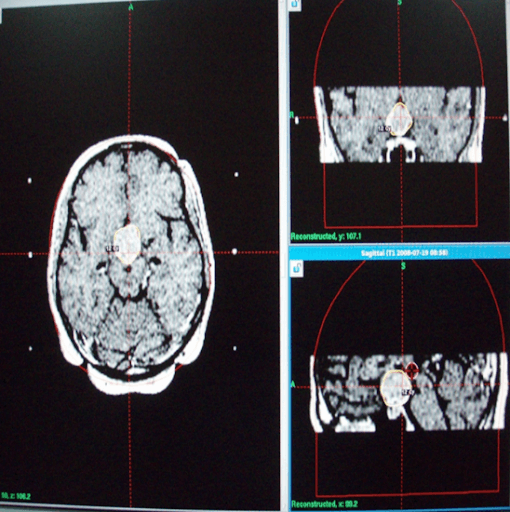
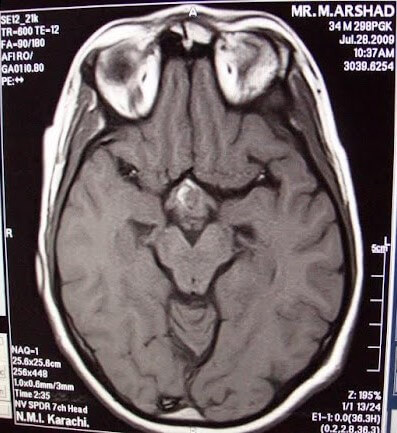
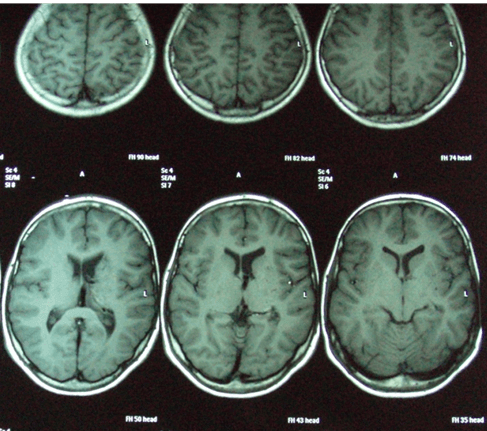
PATIENT 1
- Male 32 years old
- H/o Headache and diminished vision more on Lt. Side.
- Lt. frontal craniotomy July 2007
- Residual Craniopharyngioma.
PATIENT 2

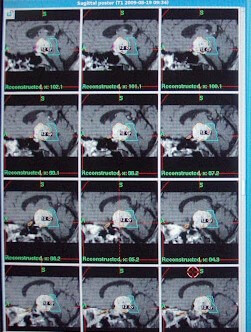
At Initial GKRS 3 months F/U 12 months F/U
RESULTS
- Mean follow up: 52 months
- Patient Outcome: Excellent in 24 (32%)
- Good in 36 (48%)
- Fair in 9 (12%)
- Poor in 6 (8%)
- Tumor control rate was 80 % and progression rate 20 %.
- No patient with normal pituitary function developed hypopituitarism after radiosurgery.
- Complete radiosurgical coverage was a significant favorable factor.
- GKRS has shown that adequate tumor control for craniopharyngiomas can be achieved if radio surgery is systematically combined with limited tumor resection, cyst drainage by neuroendoscopy and / or reservoir placement.
- Treatment related neurological deficits are rare
- GKRS FOR ARTERIO-VENOUS MALFORMATION (AVM):
-
- GKRS has been known to have excellent results in the treatments of arterio-venous malformations.
- Obliteration rates at 3- 10 years vary between 55-98% after a single procedure (dose, volume, location are the critical factors)
- Repeat SRS is required in 10-35% to achieve obliteration
- Large volume AVMs require multiple procedures
- Complications are (late cyst development, expanding hematoma) occur in 1-10% of patients
- Associated aneurysms require additional management
- Hemorrhage rates decline after SRS, approaching 1% lifetime risk after imaging confirmed obliteration
- Hemorrhage risk during the latency interval after SRS is not increased.
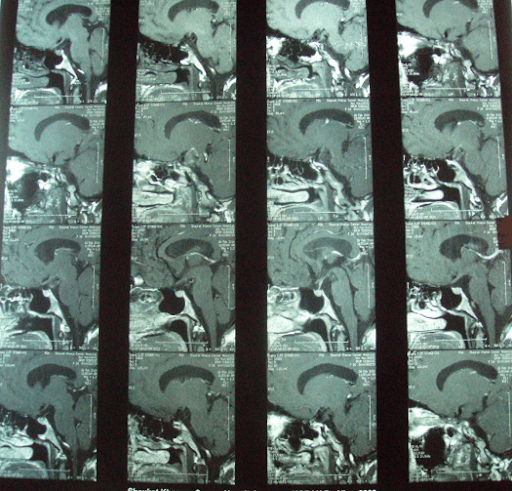
- 11-year-old male patient with a history of seizures, routine imaging a large left deep parietal AVM:
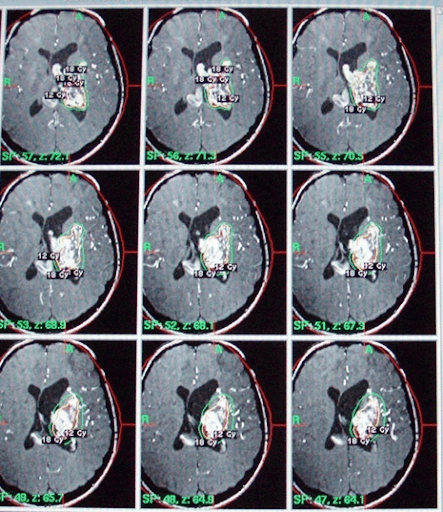
At Initial GKRS
6 Month Post GKRS
Total AVM Obliteration 1 Year Post GKRS
- THE BENEFITS OF GAMMA KNIFE RADIOSURGERY:
-
- Non-Invasive
- A variety of cerebral lesions can be treated very effectively
- May have benefits in functional brain disorders such as epilepsy, Parkinson’s disease etc.